If you’ve sought help to have a baby, there’s a good chance your health care provider has talked to you about Clomid (clomiphene). Although this oral medication has been the most widely used treatment for fertility enhancement for the past 40 years, you may still have questions about how to take Clomid to get pregnant.
Treatment with Clomid may vary depending on your needs and your health care provider. For example, Clomid treatment with a gynecologist often looks different from treatment with a fertility specialist. Sometimes Clomid is combined with other fertility treatments like intrauterine insemination (IUI). More frequently, it’s prescribed to be timed with baby-making sex at home.
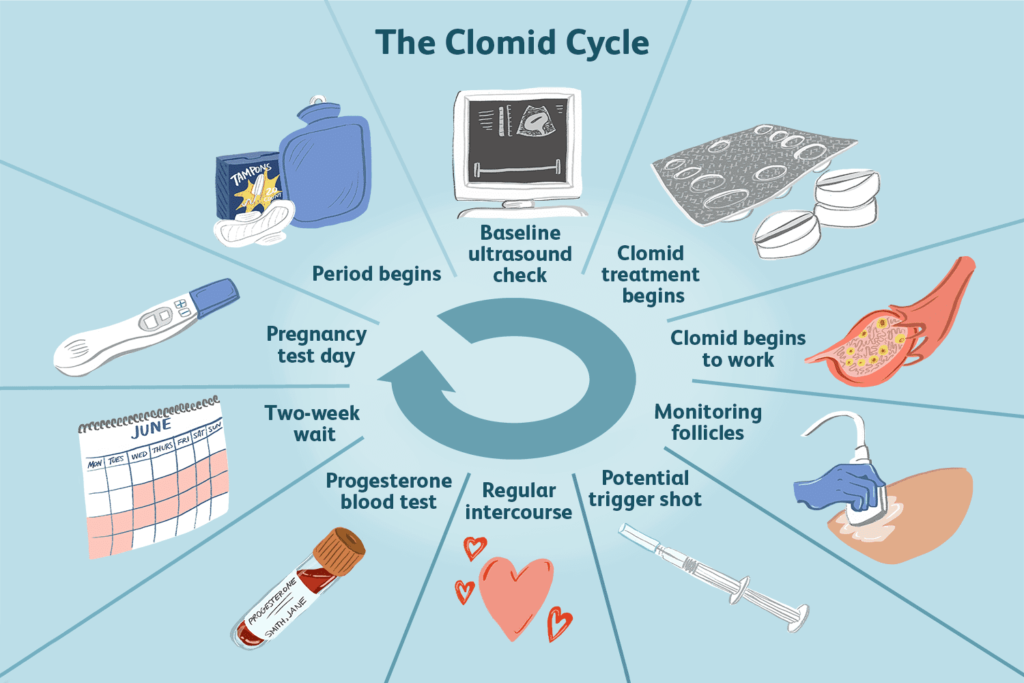
While everyone’s experience will be unique, this day-by-day guide to clomiphene treatment will give you a general idea of what to expect while taking Clomid to get pregnant.
Cycle Day 1: Your Period Begins
Day one of a cycle is the day your period begins. When it comes to fertility treatment, day one is typically marked as the first full-flow day of bright red blood before 9 p.m. If bleeding occurs after 9 p.m. or overnight, then day one is considered the next calendar day.
Take note of this date because you will need to take Clomid on particular days of your cycle. If you’re undergoing additional fertility treatments, you may also need to have certain tests done on specific days.
If you only have spotting, call your health care provider’s office. They can review your bloodwork to see where in your cycle you are.
What If You Don’t Get a Period?
If you have irregular or absent periods, your health care provider can perform a “random start” of Clomid treatment after bloodwork to check your hormone levels. If you have irregular periods, they also might prescribe the medication Provera (medroxyprogesterone), a form of progesterone. This medication will prompt your period.
Cycle Days 2–3: Baseline Ultrasound
When you call your health care provider on the first day of your cycle, you may be asked to schedule a baseline ultrasound check. A transvaginal ultrasound is done with an ultrasound probe via your vagina.
Your health care provider is looking for large cysts on the ovaries—not to be confused with the tiny cysts one might see with polycystic ovaries. Clomid can cause large cysts to grow even bigger and even rupture and bleed.
If the ultrasound reveals a large cyst, your health care provider may cancel Clomid treatment that cycle and wait to see if the cyst shrinks before starting or continuing Clomid.
Cycle Days 3–5: Start Clomid
Once your provider has cleared you, you’ll take your first dose of Clomid on the day they have instructed. You will take one dose every day for 5 days, but you won’t take any Clomid on the first day of your cycle.
Typically, people taking Clomid are given a dose of one 50-milligram pill once daily for 5 days. Your health care provider may tell you to take the Clomid pills on one of the following sequences:
- On cycle days 2, 3, 4, 5, and 6
- On cycle days 3, 4, 5, 6, and 7
- On cycle days 5, 6, 7, 8, and 9
Your health care provider might recommend taking Clomid at the same time every day. Some say that taking the pill before bed can help you sleep through some of the side effects, which may include hot flashes, bloating, and sore breasts. Others do better if they take the pill in the morning.
Cycle Days 3–9: Clomid Begins to Work
You won’t ovulate during the five days you’re taking Clomid pills. However, with your first dose, Clomid begins a chain reaction that will eventually lead to ovulation. In a successful cycle with the medication:
- Clomid binds to certain receptors in your brain to signal that the body is too low in estrogen.
- This causes the brain to produce more follicle-stimulating hormone (FSH), which boosts estrogen and prompts eggs to mature in your ovarian follicles.
- Once mature, at least one of these eggs will be released from your follicles into your fallopian tubes to be fertilized by sperm.
Cycle Days 10–21: Monitor Follicular Growth
Beyond suggesting that you use an ovulation predictor kit so you can time baby-making sex for your most fertile days, most OB-GYNs don’t carefully monitor Clomid treatment cycles. But many reproductive endocrinologists do. Fertility doctors monitor Clomid cycles for two primary reasons:
- To see how many follicles grow: If more than two or three appear, you’re at high risk for pregnancy with twins or higher-order multiples. Your provider will want to discuss the possibility of canceling that particular cycle (by avoiding penis-in-vagina sex or further fertility treatments).
- To time a “trigger shot” of human chorionic gonadotropin (hCG): This trigger shot can prompt an egg to finish maturing and burst from the ovary.
- To time intercourse or intrauterine insemination (IUI): Knowing when you’re about to ovulate can help you have baby-making sex or an IUI during your most fertile window.
Monitoring the cycle usually starts a few days after your last Clomid pill is taken and may involve ultrasounds and bloodwork every few days until you ovulate. The ultrasound technician will measure the growing follicles, and your health care provider will decide based on their growth when to time a trigger shot (if you’re having one), intercourse, or an IUI.
Cycle Days 15–25: Trigger Shot
If you’re seeing a fertility specialist, they may prescribe an injection of the hormone human chorionic gonadotropin (hCG), also known as a “trigger shot,” during your Clomid cycle. It’s called a trigger shot because it triggers ovulation to occur within 24 to 36 hours. Your health care provider may order a trigger shot to help better time for IUI or intercourse or to give your ovaries a little extra boost.
If you’re receiving a trigger shot, providers will typically administer it seven to nine days after your last Clomid pill. But if ultrasound monitoring finds that your eggs need more time to mature before getting kicked out of their cozy follicle beds, your doctor may wait a bit longer.
If you’re given a trigger shot, be aware that a pregnancy test taken within a week of the shot may register as positive, even if you aren’t pregnant. The test will pick up on the hormones given via the injection.
Cycle Days 10–17: Timed Intercourse/IUI and Ovulation
Ovulation typically occurs 5 to 10 days after taking the last Clomid pill. So if you took Clomid on days 3 to 7 of your cycle, you are most likely to ovulate between days 10 and 16. If you took Clomid on days 5 through 9, ovulation is most likely to occur between days 12 and 17 of your cycle. If you were given a trigger shot, then ovulation will occur 24 to 36 hours after the injection.
When To Have Sex During Clomid Cycle
Unless your health care provider tells you otherwise, you should have baby-making sex every other day or every day starting three days after you take your last Clomid pill. You should continue having sex until you have confirmed that ovulation occurred.
If you are doing an IUI cycle, on the other hand, your health care provider will tell you when to come in for the IUI based on your ultrasounds and the timing of your trigger shot. In most cases, you can also have sex on your fertile days at home in addition to your scheduled IUI.
Cycle Days 19-21: Progesterone Blood Test
Both gynecologists and fertility specialists typically order a progesterone blood test to confirm you’ve ovulated sometime between cycle days 19 and 21. It may be later if your provider knows you’ve ovulated later than day 21 of your cycle.
Progesterone is a hormone that rises after ovulation, and testing for it can confirm whether or not Clomid successfully triggered ovulation. Also, if your progesterone levels are too low, your health care provider may order a progesterone vaginal suppository. Healthy progesterone levels prepare the uterine lining for a fertilized egg to implant and start developing.
Cycle Days 21–35: The Two-Week Wait
The two-week wait begins after you ovulate and ends either with a positive pregnancy test or your period. This wait is probably the hardest part of the cycle to endure. All you can do is be patient and see if the Clomid cycle worked.
You may have some bloating as your ovaries are hard at work. Severe cases of ovarian hyperstimulation syndrome (OHSS), which can cause fluid from your ovaries to leak into your belly and chest, are rare if you’re taking Clomid alone. However, the risk rises if you pair it with fertility treatments. Let a doctor know if you have severe bloating or discomfort.
Some menstruating people confuse the bloating from the Clomid-stimulated ovaries with an early pregnancy symptom. Some of the side effects of Clomid can mimic pregnancy symptoms. Remember feeling pregnant doesn’t mean you are pregnant, especially when using fertility medications.
Cycle Days 28–35: Pregnancy Test
Finally, the day you waited for all month: pregnancy test day. Your health care provider may order a beta pregnancy test (a blood test that measures the amount of hCG in your blood) in the middle of your two-week wait and at the end. Or, they may order blood work only at the end.
It’s also possible they will simply ask you to take an at-home pregnancy test sometime between days 28 and 35 of your cycle and instruct you to call if you get a positive result.
If the test is positive, congratulations! Your health care provider will likely monitor the pregnancy for a few weeks to be sure everything is going smoothly and to check if you have conceived twins. If you’re more nervous than excited, that’s normal. Pregnancy after fertility challenges can cause a wide range of emotions.
What Happens If the Clomid Cycle Fails
If your pregnancy test is negative, your health care provider may wait and retest you again. It’s possible the pregnancy hormone levels are not high enough yet. If you get your period while waiting to test again, the treatment probably didn’t work that cycle.
Having an unsuccessful cycle can be upsetting, and it’s common to feel defeated and lose some hope. Remember that you can try again and that sometimes treatment needs adjustments before you reach success.
How your health care provider addresses a failed Clomid cycle will depend on your situation. Every case will be different, but here are some possible scenarios.
No changes
Your doctor may recommend another cycle of Clomid at the same dose, especially if you successfully ovulated but did not get pregnant. Just because the cycle didn’t lead to pregnancy doesn’t necessarily mean anything about your treatment should be adjusted right away. It may work on the next try.
Higher dose
If you didn’t ovulate, another cycle of Clomid at a higher dose may be the next step. The first cycle of Clomid is typically started at 50 milligrams, but many people won’t ovulate at that dosage. If this happens to you, the dosage may be increased.
Your health care provider will probably keep trying higher dosage levels until a certain point, after which other treatments might be considered. Doctors may suggest switching to an alternative ovulation-stimulating drug (letrozole) or taking Clomid along with metformin, a diabetes drug often used to trigger ovulation in people with polycystic ovarian syndrome (PCOS).
New treatment options
If several cycles of Clomid don’t lead to pregnancy, new treatment options may be considered. By six cycles, Clomid use is linked to health problems for both parents and babies.
Tip
While this day-to-day guide to taking Clomid to get pregnant can give you a general sense of what you can expect with Clomid treatment, everyone’s fertility journey is different. If you have been prescribed Clomid, it’s important to follow your health care provider’s instructions. They can advise you on what treatments and timelines are best for you.